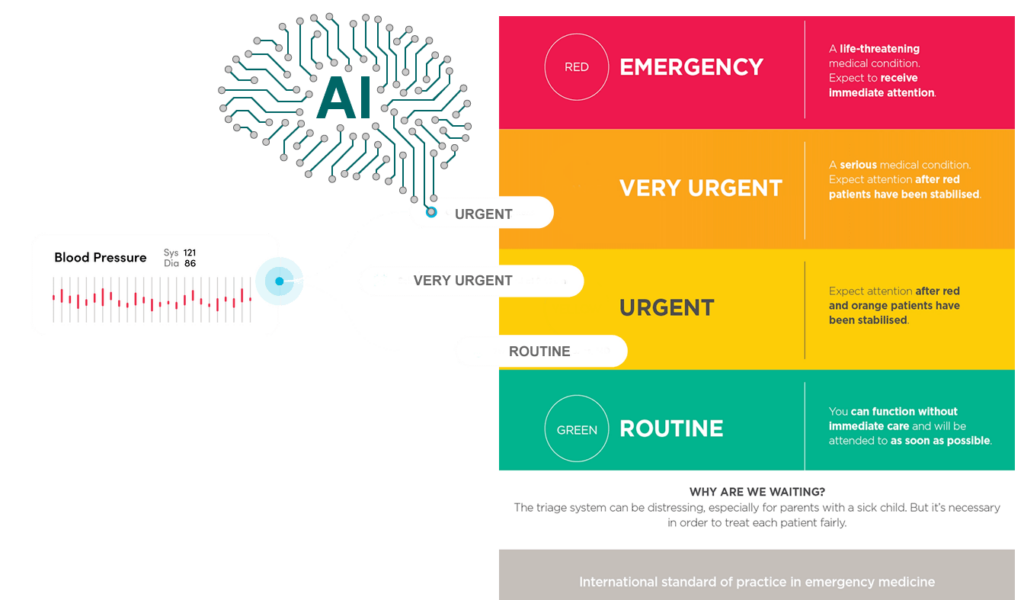
In today’s rapidly evolving healthcare landscape, effective patient care is crucial. Triage prioritizes treatment based on the severity of conditions. It is a cornerstone of modern medical practice. Triage helps healthcare systems manage high patient volumes and limited resources efficiently. This process ensures high-quality care. It is essential in emergency settings, outpatient clinics, and large-scale disaster responses.
1. Improving Resource Management in Healthcare Systems
Triage optimizes limited healthcare resources. Hospitals and clinics operate under significant pressure. This is especially true in growing populations or health crises like COVID-19. Resources such as medical staff, equipment, and beds are limited. Demand often exceeds supply.
Triage allows healthcare professionals to quickly assess patients. They can determine the level of care each individual needs. This prevents overutilization of resources by patients with minor conditions. Those in critical need receive immediate attention. For example, a patient with chest pains indicative of a heart attack will get prompt intervention. In contrast, a patient with a sprained ankle might be treated later or referred to outpatient services. This prioritization maintains a balanced system where resources are allocated effectively.
Triage also prevents the misuse of specialized resources. Without a strong system, non-urgent cases could occupy critical areas. This would leave no space for patients needing life-saving procedures. By ensuring appropriate resource use, triage maintains healthcare facilities’ functionality.
2. Reducing Waiting Times and Delivering Faster Care Through Triage
Waiting times are common in emergency departments and other high-pressure environments. Without triage, all patients would be treated in the order they arrive, regardless of urgency. This could lead to catastrophic outcomes, especially for those in life-threatening situations.
Implementing triage helps healthcare providers identify and prioritize urgent needs. This ensures that patients with critical conditions, like heart attacks or severe trauma, receive timely treatment. For less severe cases, triage sets realistic expectations about wait times, reducing anxiety.
Research shows that triage significantly reduces average waiting times. A 2020 study by the National Institute of Health found that hospitals using a comprehensive triage system experienced a 30% reduction in wait times during peak hours. This efficiency improves patient outcomes and satisfaction.
3. Preventing Overcrowding and Enhancing Patient Experience
Overcrowding in hospitals, particularly in emergency departments, affects care quality. Without proper management, emergency rooms can become overwhelmed by non-urgent cases. This leads to long wait times and delays in treating serious conditions.
Triage prevents overcrowding by classifying patients based on severity. Individuals with life-threatening issues are seen immediately. Others with less critical problems may be directed to outpatient care or scheduled appointments. For example, a patient with flu-like symptoms might be referred to a primary care physician, freeing emergency resources for urgent cases.
Triage also helps prevent infection spread in hospitals. By identifying and isolating contagious patients early, healthcare providers limit exposure, improving overall safety and efficiency.
4. Minimizing Unnecessary Medical Tests and Procedures
Triage reduces the number of unnecessary medical tests and procedures. Patients may present symptoms that suggest serious conditions but do not require extensive diagnostic work. For instance, a patient with mild chest discomfort might not need immediate cardiac catheterization. A stress test or ECG may suffice.
Evaluating symptoms and medical histories allows triage to inform decisions on necessary tests. This reduces strain on diagnostic services, ensuring resources are available for patients who truly need them. It also minimizes unnecessary radiation exposure or invasive procedures, contributing to better health outcomes.
5. Enhancing Quality of Care Across Different Settings
Triage benefits various healthcare environments, including urgent care clinics and during public health crises. It streamlines patient assessments and interventions, ensuring timely care.
In outpatient settings, triage manages high volumes during flu season. Patients with mild symptoms may receive advice over the phone or through online consultations. This frees up clinic appointments for complex needs.
During public health emergencies like pandemics, triage is essential for prioritizing care. During COVID-19, hospitals implemented triage systems to manage surges, ensuring critical cases received timely treatment.
6. Supporting Healthcare Workers and Reducing Burnout
Healthcare workers face immense pressure when treating large numbers of patients. Triage benefits patients and alleviates medical staff workload. It allows focus on urgent cases without overwhelming providers.
Burnout among healthcare workers is a significant issue, especially in emergency rooms. A study published by the Journal of Emergency Nursing found that effective triage reduces burnout. It organizes patient care more efficiently, allowing medical professionals to manage time and resources better. This leads to improved well-being for healthcare workers and better patient outcomes.
7. Managing Mass Casualties and Large-Scale Emergencies
Triage is crucial in mass casualty situations, such as natural disasters or terrorist attacks. Healthcare providers must make tough decisions about whom to treat first, often with limited time and resources. The goal is to maximize lives saved by prioritizing those likely to benefit from immediate intervention.
For example, after an earthquake, triage might prioritize patients with severe injuries, like internal bleeding, while those with less serious injuries might wait. This approach ensures care is provided where needed most, even in chaotic situations.
8. Time Management for Non-Emergency Cases and Routine Care
Triage improves time management in non-emergency settings. In outpatient clinics or primary care practices, it helps schedule appointments and allocate resources efficiently. Patients with chronic conditions can be seen regularly, while those with acute symptoms receive immediate attention.
This system ensures effective time management, leading to better outcomes and efficient resource use. It allows patients to receive care without long waits, improving satisfaction with the healthcare system.
Conclusion
Triage is a critical component of modern healthcare. It manages limited resources, reduces waiting times, prevents overcrowding, and ensures patients receive appropriate care. Its importance is particularly evident in emergency settings and public health crises. As healthcare systems face increasing demands, triage remains essential for delivering high-quality, patient-centered care.
References
- American College of Emergency Physicians (ACEP). (2023). “The Role of Triage in Emergency Medicine.”
- World Health Organization (WHO). (2022). “Healthcare Systems and Triage Management.”
- National Library of Medicine. (2021). “Emergency Triage: A Vital Process for Healthcare Systems.”
- Journal of Emergency Nursing. (2020). “The Impact of Triage Systems on Healthcare Worker Burnout.”